Table of Contents
What Are Non Cardiac Chest Pain Symptoms?
Introduction
Chest pain can be a frightening experience, sending shivers down your spine and triggering anxieties about a heart attack. While chest pain can be a symptom of a heart attack, it’s important to remember it can also stem from numerous non-cardiac (non-heart related) causes. Understanding these non-cardiac causes empowers you to differentiate them from heart-related issues and make informed decisions about your health.
Beyond The Heart: Exploring Non-Cardiac Causes Of Chest Pain
The human chest houses various organs and structures, making it susceptible to discomfort arising from diverse sources. Here are some common non-cardiac causes of chest pain:
-
Musculoskeletal Pain:
This is a frequent culprit for chest aches. Muscles, ligaments, and tendons in the chest wall can become strained or inflamed due to poor posture, repetitive movements, or injuries like a pulled muscle. This pain is often localized to a specific area and might worsen with specific movements like coughing or deep breaths.
-
Costochondritis:
This condition involves inflammation of the cartilage that connects your ribs to your breastbone. It can cause a sharp or dull ache in the chest, often worsened by deep breaths, coughing, or pressing on the affected area.
-
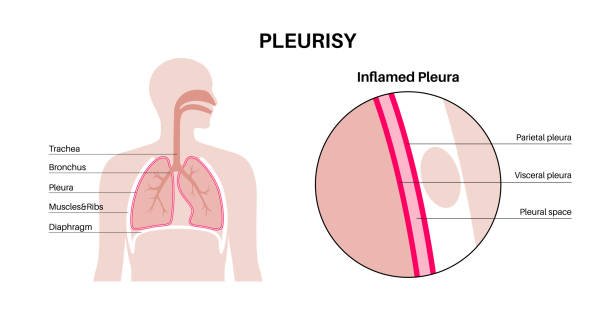
Pleurisy:
This is the inflammation of the pleura, the thin lining that separates your lungs from your chest wall. Pleurisy can cause a sharp or dull ache in the chest that worsens with each breath, coughing, or laughing. You might also experience shortness of breath.
-
Gastroesophageal Reflux Disease (GERD):
GERD occurs when stomach acid backs up into the esophagus, causing heartburn, a burning sensation in the upper chest or abdomen. However, GERD can also manifest as a dull ache in the chest, often accompanied by a sour taste in the mouth or difficulty swallowing.
-
Anxiety and Panic Attacks:
Anxiety and panic attacks can trigger various physical symptoms, including chest tightness, discomfort, or a dull ache in the chest. This discomfort typically comes on suddenly, subsides within minutes, and doesn’t worsen with activity.
-
Shingles:
This viral infection can cause a burning or stinging pain along the path of affected nerves, sometimes including the chest area. Shingles pain can be present even before the characteristic rash appears.
Differentiating Non-Cardiac from Cardiac Chest Pain
While both cardiac and non-cardiac chest pain can be concerning, certain characteristics can help distinguish them:
| Feature | Non-Cardiac Chest Pain | Cardiac Chest Pain |
| Location | Can occur anywhere in the chest | Often felt in the center of the chest, radiating to arms, jaw, neck, back |
| Nature of Pain | Sharp, stabbing, burning, aching, tightness | Crushing, squeezing, pressure |
| Triggers | Specific movements, posture, foods (GERD), anxiety | Often no identifiable trigger, exertion might worsen |
| Duration | Variable (fleeting to persistent) | Often persistent, unrelieved by rest or medication |
| Accompanying Symptoms | May include cough, difficulty swallowing, sour taste | May include shortness of breath, sweating, nausea, vomiting |
Remember: This is a general comparison, and exceptions might exist. If you experience any concerning chest pain, seek medical attention for a proper diagnosis.
Additional Tips For Managing Non-Cardiac Chest Pain
-
Identify Potential Triggers:
Reflect on activities, foods, or medications that might be triggering the pain. Avoiding such triggers can help manage the discomfort.
-
Over-The-Counter Pain Relief:
Medications like ibuprofen or acetaminophen can help alleviate pain caused by musculoskeletal issues or GERD. Always consult your doctor before taking any medication.

-
Home Remedies:
Applying a heating pad or warm compress to the affected area can provide temporary relief for muscle aches.
-
Stress Management Techniques:
Techniques like deep breathing exercises, meditation, or yoga can help manage anxiety-related chest pain.
-
Maintain Good Posture:
Poor posture can strain chest muscles, so practicing good posture throughout the day can help prevent future aches.
Frequently Asked Questions (FAQs)
-
Can A Lung Infection Cause Chest Pain?
Yes, a lung infection like pneumonia can cause a dull ache or sharp pain in the chest, often accompanied by fever, cough, and shortness of breath.
-
Should I Go To The Emergency Room For Heartburn?
Severe or persistent heartburn can be a sign of an underlying condition. If over-the-counter medications don’t provide relief or you experience frequent heartburn, consult your doctor. However, for occasional heartburn, you don’t necessarily need an emergency room visit.

-
What If My Chest Pain Feels Like Tightness Or Pressure?
Tightness or pressure in the chest can be caused by various factors, including anxiety, GERD, or angina (a symptom of heart disease where reduced blood flow causes chest discomfort). If you’re unsure about the cause, especially if accompanied by other symptoms like sweating, shortness of breath, or lightheadedness, seek medical attention to rule out any serious conditions.

-
Can I Prevent Non-Cardiac Chest Pain?
While you can’t entirely eliminate the risk of non-cardiac chest pain, certain lifestyle practices can help:
-
Maintaining A Healthy Weight:
Excess weight can put strain on the chest wall muscles, contributing to pain.
-
Regular Exercise:
Exercise strengthens muscles and improves overall health, reducing the risk of musculoskeletal pain.
-
Managing Stress:
Stress can exacerbate chest pain triggered by anxiety or GERD. Practicing stress management techniques can be beneficial.
-
Eating A Healthy Diet:
A balanced diet rich in fruits, vegetables, and whole grains can help manage GERD and promote overall well-being.
-
Conclusion
Chest pain can be a source of worry, but understanding the distinction between cardiac and non-cardiac causes empowers you to manage the discomfort effectively. Non-cardiac chest pain, while potentially concerning, often arises from treatable conditions. By recognizing the characteristics of non-cardiac pain, identifying potential triggers, and adopting healthy lifestyle practices, you can minimize the frequency and severity of these episodes.
However, it’s crucial to remember that this information shouldn’t replace professional medical advice. If you experience any concerning chest pain, particularly if it’s accompanied by shortness of breath, sweating, nausea, or radiating discomfort, don’t hesitate to seek immediate medical attention. Early evaluation can ensure proper diagnosis and treatment, promoting optimal health and well-being.
References
- American College of Rheumatology: Provides information on musculoskeletal conditions like costochondritis.
- National Heart, Lung, and Blood Institute: Offers information on pleurisy, its causes, and symptoms.
- National Institute of Diabetes and Digestive and Kidney Diseases: Provides detailed information on GERD, its symptoms, and treatment options.
- Anxiety and Depression Association of America: Offers information on anxiety symptoms, including physical manifestations like chest pain.
- Mayo Clinic: Provides a comprehensive overview of chest pain, including differential diagnoses and treatment options.
Discover more from Pain Relief Methods
Subscribe to get the latest posts sent to your email.
